 |
Talk To or Communicate With - Email in Medical Care
|
|||
|
||||
Introduction
Back to the Table of Contents
The entire structure of successful healthcare rests upon accurate communication between the caregivers and those being cared for. This bond begins at the instant the person seeking help contacts and communicates with the initial person of the caregiver system.
The Merriam-Webster dictionary defines communication as; "interchange of thoughts or opinions through shared symbols." The phrase shared symbols is always the key to real communication. An analysis of this connection between persons says that if you cannot tell me what I told you in a fashion that I understand it is what I thought I told you then we have never communicated! We may have made noises between us or exchanged written symbols but no matter in what form we contacted each other we did not communicate.
I cannot number the times I have asked a patient, "What did I just tell you?", and have them either be speechless or haltingly give some answer which did not contain what I thought I told them. In those instances I had not communicated with the patient! If I had not asked them for the repeat of what I told them I would have never known I was unsuccessful in communicating with them!
Since this possible gap in communication exists how does one circumvent it? If one is face to face with the person the question about "what did I just tell you" works well. However if the communication is at a distance, such as telephone then, unless the person is a very close acquaintance and not easily offended, the blunt asking of such a question may be offensive or irritating. Therefore the best answer for such remote communication is a written document that can be read and re-read by the recipient. If the reader does not understand the document they can call the sender and since both have the same document a discussion can be held over the contents of the document until both parties agree upon the meaning. Then the parties have communicated!
Caregivers in the field of medicine or other have used informational pamphlets for years to help in this communication problem. These are printed documents whose content has been designed to communicate. Thus there is a long history of using formatted documents for this purpose.
What is email but a written, formatted document? Such a communication can contain graphics thought to be a help in communicating the subject in question. The recipient can read and re-read this document and if necessary contact the sender verbally to definitively understand the symbology such that sender and recipient both agree on the meaning of the message. Clearly then email is better for communication than the telephone! The only possible advantage of the telephone is instant feedback. However, since reception of real meaning can't easily be queried then that instant feedback is of little use.
If email seems to be such a good medium of communication with a patient why is it not used more extensively? The answer to such a question revolves around responsibility. The responsibility questions initiate with a question on whether or not an exchange of email generates a physician-patient contract with all that goes with that in the realm of liability. There is now with the implementation of HIPAA (Health Insurance Portability and Accountability Act) a new player in the realm of physician-patient communication. This HIPAA has standards that must be met and regulations that must be followed.
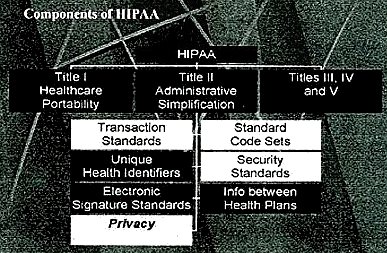
This 2001 graphic from the Oregon Medical Association of some of the facets of HIPAA illustrates the complexity of this new government system. The most important area of HIPAA relating to email communication is privacy.
Now that we have mentioned responsibility and privacy as major factors in planning for email communication with patients some published comments on these problems will be reviewed.
Responsibility and Privacy
Back to the Table of Contents
-
A discussion of responsibility revolves around the concept that a healthcare provider is responsible for communicating concepts of diagnosis and treatment to a patient and in some way certifying that was done. However there is no requirement for a certification that the patient understands the concepts. Patients are asked to read and sign numerous documents relating to their therapy and their contacts, professional and business, with the healthcare system. Many of these documents have language such that when the patient signs the document he or she is certifying that they understand and agree with the contents of the document.
The American College of Surgeons did a very interesting study several years ago. Patients scheduled to undergo serious major surgery had a pre-operative conference discussing the details of the coming surgery including the expected outcomes and the possible hazards and risk. This conference was videotaped. Six weeks after the surgery they were interviewed again and asked if the surgery and its post-operative course was what had been discussed with them before surgery. A very significant percentage of those patients did not remember what had been discussed and were surprised when they were shown the video. This study is an important illustration of possible problems with patient understanding of medical events. Documented email information exchanges in the medical record illustrating a significant effort toward patient understanding would be beneficial to all.
Comprehension of communication can be a major problem in the responsibility area. However, the first decision in this area is to decide a time frame of communication that is appropriate for email communication. It is not appropriate to communicate regarding healthcare problems that fall into a category requiring urgent care. Email by its very nature is a delayed communication. The message is sent through multiple electronic systems before arriving at its destination. In most cases the recipient of an email does not access and read email continuously. Email is most usually accessed and read at a time convenient to the reader. This ability to read email at a time of convenience is one of the good points of email. However, since a significant time may happen between receipt of the email in a computer system and its being read it is not appropriate for items of urgent care. It is very important to make sure patient users of email understand this and to document that they understand this limitation of email. This limitation of email is commented on in several publications. 1,2,3,4,5 Doctor Kane and Sands article begins with some excellent beneficial aspects of email 4 -
1. E-mail follow-up allows retention and clarification of advice provided in clinic.
2. E-mail creates a written record that removes doubt as to what information was conveyed.
3. E-mail is especially useful for information the patient would have to commit to writing if it were given orally.
4. E-mail messages can embed links to educational materials.
5. E-mail messages are less likely to accidentally fall through the cracks of a busy practice.
6. In contrast with telephone conversations, e-mail is self-documenting. - There is a little mantra of defensive medicine which alludes to never getting sued for the records you keep but getting sued for records you did not keep. Properly archived e-mail added in as part of the regular medical record helps to complete the medical record in the area of physician-patient communication.
The observations in the AMA Guidelines5 support these benefits. - 1. E-mail allows for follow-up patient care and clarification of advice provided in a professional office setting.
2. E-mail creates a written record that removes doubt as to what information was conveyed.
3. Some frequently used patient handouts can be ported to e-mail.
4. E-mail messages can embed links to educational materials and other resources on the clinician's web site or on other Internet sites.
- The excellent guidelines for HIPAA by Dr. Rada 1note that, "An email policy is not required by the Privacy Rule." However this section goes on and gives some advice for an e-mail policy.
- 1. Confidentiality: When e-mail is used for communication of individually
identifiable health information a notation referring to the confidential nature
of the information should be made in the subject line.
2. Some e-mail may be considered a formal record and should be retained.
3. The information is to be distributed only to those with a legitimate need to know.
4. All clinically relevant e-mail messages, including the full text of a patient's query, as well as the reply, should be stored in the patient's medical record. - The comprehensive AMA Guidelines5 define physician-patient email, "Patient-physician electronic mail is defined as computer-based communication between physicians and patients within a professional relationship, in which the physician has taken on an explicit measure of responsibility for the patient's care."
This document then has Communication Guidelines: - 1. Establish turnaround time for messages.
2. Inform patients about privacy issues (and document this)
3. Patients should know who besides addressee processes messages during addressee's usual business hours and during addressee's vacation or illness.
4. Physicians should retain electronic and/or paper copies of e-mails
5. Establish types of transactions (prescription refill, appointment scheduling, etc) and sensitivity of subject matter (HIV, mental health, etc) permitted over e-mail.
6. Instruct patients to put the category of transaction in the subject line of the message for filtering and appropriate routing.
7. Request that patients put their name and patient identification number in the body of the message.
8. Configure automatic reply to acknowledge receipt of messages.
9. Send a new message to inform patient of completion of request.
10. Request that patients use autoreply feature to acknowledge reading the clinician's message.
11. Develop archival and retrieval mechanisms.
12. Maintain a mailing list of patients, but do not send group mailings where recipients are visible to each other to each other. Use blind copy feature in software.
13. Avoid anger, sarcasm, harsh criticism, and libelous references to third parties in messages.
14. Append a standard block of text to the end of e-mail messages to patients, which contains the physician's full name, contact information, and reminders about security and the importance of alternative forms of communication for emergencies.
15. Explain to patients that their messages should be concise.
16. When e-mail messages become too lengthy or the correspondence is prolonged, notify patients to come in to discuss or call them.
17. Remind patients when they do not adhere to the guidelines.
18. For patients who repeatedly do not adhere to the guidelines, it is acceptable to terminate the e-mail relationship.
Medicolegal and Administrative Guidelines:
Back to the Table of Contents
- 1. Develop a patient-clinician agreement for the informed consent for the use of e-mail. This should be discussed with and signed by the patient and documented in the medical record. Provide patients with a copy of the agreement. Agreement should contain the following
-
a. Provide instructions for when and how to convert to phone calls and office visits.
b. Describe security mechanisms in place
c. Hold harmless the health care institution for information loss due to technical failures.
d. Waive encryption requirement, if any, at patient's insistence
e. Details of security mechanisms in place:
1) Using a password-protected screen saver for all desktop workstations in the office, hospital and at home.
2) Never forwarding patient-identifiable information to a third party without the patient's express permission
3) Never using patient's e-mail addresses in marketing schemes.
4) Not sharing professional e-mail accounts with family members
5) Not using unencrypted wireless communication with patient- identifiable information.
6) Double checking all "To" fields prior to sending messages
7) Perform at least weekly backups of e-mail onto long-term storage. Define long-term as the term applicable to paper records.
8) Commit policy decisions to writing and electronic form.
- The study by Patt, et al2 has some interesting observations about doctors using email with their patients.
- 1. The physicians surveyed believed that e-mail saves time spent in tracking
patients down by telephone.
2. E-mail allows more opportunity for patients to communicate during a busy workday and after hours.
3. Some physicians believe that e-mail has a positive effect on the doctor-patient relationship by increasing rapport and communication.
4. Most physicians felt there was great potential for exchange of educational information and management of chronic diseases.
5. However re-imbursement for the time and effort of using e-mail was seen as a problem. It takes significant time and effort and resources to compose and send e-mail. The physicians surveyed felt that if commensurate payment for this effort was not possible then e-mail would only rarely used. - The article of Morlang3 noted that business consultants felt that a 15 minute e-mail consultation with a patient is worth about $57.00. However, the experience of Government projects in rural medicine notes that e-mail may not be interactive and thus not reimbursable. The article by Kane, et.al4 and the AMA Young Physicians guidelines make no mention of possible reimbursement. It is interesting that e-mail consultation with an attorney is billed at a carefully calculated amount determined by the cost of the attorney's billable hour and the time spent to deal with any effort associated with evaluating a received e-mail or sending an e-mail.
Now that commentary has been made on guidelines for the use of e-mail in clinical medical practice and a brief mention has been made on the possibility of charging for the service the next and perhaps most important areas or discussion concern privacy and security.
Critical Concepts
Back to the Table of Contents
- Before discussing technical details of these two subjects it is important to refer to the excellent discussion of HIPAA by Dr. Rada. He notes that there are some critical concepts to learn.
- 1. Covered Entity: A healthcare provider, a health plan, or a clearinghouse
is a covered entity. HIPAA compliance is required of covered entities.
2. Individually identifiable health information: Any health information about a patient that includes the name, phone number, address, social security number, or other such identifier is considered individually identifiable health information.
3. Protected health information: Individually identifiable health information in a covered entity that has at any time had any such information in electronic form in HIPAA transaction (such as a claim or eligibility inquiry).
4. Uses and Disclosures: Use occurs when a person within covered entity shares protected health information with another person inside the same covered entity, whereas disclosure occurs when the information goes from one entity to another.
- Dr. Rada notes in that, "An email policy is not required by the Privacy Rule". However he does discuss some salient points an email policy could contain. Since the above critical concepts apply to any healthcare provider it would seem prudent to have a well planned and extensive policy. Any well planned policy needs to discuss privacy and confidentiality.